[ad_1]
LAMU ARCHIPELAGO, Kenya ― The motor sputters to life, kicking up saltwater and spitting a cloud of exhaust into the pre-dawn stillness.
The captain and his deputy help two doctors from Nairobi, three medical assistants and a nurse climb aboard. They cram themselves among the waterproof boxes packed with vaccines and sterile equipment. As daylight breaks, they’re speeding northeast along the Indian Ocean coast toward some of Kenya’s poorest and most isolated villages, where there are few doctors and locals have little access to health care.

The team is part of Safari Doctors, a nonprofit that makes monthly trips deep into the Lamu Archipelago on Kenya’s dazzlingly beautiful northern coast. The word “safari” means “to travel” in East Africa’s Swahili language ― and the dozen or so villages the team visits on each trip require a difficult journey. To reach their first destination, the mainland village of Kiangwe, they weave the boat through a maze of channels, mangrove forest and white sand beaches for two hours, then set up a makeshift clinic and treat as many people as they can before moving on, zigzagging across the sea and camping out under the stars for several nights.
“Safari Doctors are the only doctors we see,” said Fatuma Ahmed, 24, a mother of a wailing baby girl, waiting to see the medics in Kiangwe. The nearest hospital is days away ― too far to reach on her own, she said.
Since 2015, the Safari Doctors group has served a population of subsistence farmers, fishers and herders in a region that borders war-torn Somalia. Regular attacks inside Kenya by the Somali-led militants known as al-Shabab frightened off many of the doctors in Lamu County. Clinics have closed, leaving villagers without the tools they need to avoid diseases such as leprosy and polio. For some of the locals who came to meet the team on their October trip, these free monthly pop-up clinics are the difference between life and death.
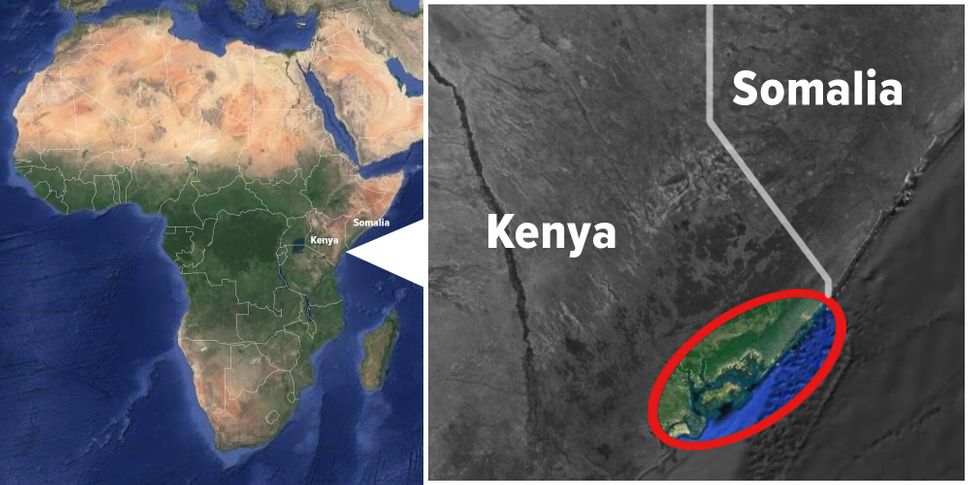
“We could walk to Somalia from here,” Harrison Kalu, the team’s nurse, told HuffPost as he carefully put two drops of polio vaccine into the mouth of a crying toddler in Kiangwe. Somalia has struggled to contain a polio outbreak due to low vaccine coverage. The disease spreads quickly among unvaccinated children and can cross country borders with human travelers, warns the World Health Organization. Under these circumstances, the WHO recommends that health professionals in Kenya monitor vulnerable communities and keep distributing vaccines.
“Without vaccinations, people would really suffer,” said Kalu, 67, a former member of the Kenyan navy who has worked as a nurse for almost 50 years. As a staffer for Safari Doctors, he directs the organization’s teams in the field.
It is not only children they help. Everyone from the villages comes to the clinics when the doctors arrive.
“My hands are too sore to work,” said fisherman and farmer Mohammed Adan, showing an infected wound from when he cut himself while hoeing his fields. “If I can’t work, my family will go hungry.”

Kalu and his team can see as many as 800 patients on each sailing trip. They stop for only a few hours in each village, setting up their gear inside crumbling community halls or thatch-roof buildings. Outside, families wait in snaking lines for a checkup. In Kiangwe, HuffPost observed that several of the patients who arrived at the clinic were soldiers from Kenya’s army, posted in bush forts to defend against the al Qaeda-aligned al-Shabab insurgents.
Al-Shabab guerrillas, fighting to establish an Islamist state, made international headlines in 2013 for attacking the Westgate shopping mall in Nairobi, killing dozens. But the group had been active in Lamu County in years prior: In 2011, militants kidnapped a French vacationer on Manda Island ― a destination for wealthy foreign tourists. Numerous violent incidents rocked the county for the next several years.
“It was terrifying for my family,” said Faisal Abdi, a farmer and patient at one of the clinics, talking of the times five years ago when al-Shabab was at its most dangerous. “We had to run and hide when the fighting came close.”
Kenyan military forces have pushed much of the insurgent force out of the rural areas and across the border into Somalia.
“These days, things are better, as the army has bases close by,” added Abdi. “But still they [the militants] hide in the forests close by.”

The threat from al-Shabab is not completely gone, and the remaining militants know that teams from Safari Doctors visit this area, Kalu told HuffPost.
In one raid on a village the doctors visit, when they stole equipment left by the team for its next trip, the militants asked the community where Kalu the nurse was. “They asked for me by name,” Kalu said.
Still, he said he isn’t ready to stop coming because the need is so great.
When the violence was at its peak, the local government did what it could to keep medical clinics staffed ― but the Lamu region now has only 10 doctors serving about 150,000 people, according to Safari Doctors.
“Due to the security situation, people did not feel safe to be in some of the areas, so some services closed,” said Dr. Victor Tole, chief officer for medical services in the Lamu government. “People had no other alternative for health care.”
The dearth of rural doctors means that local health workers, who have some medical training (often informal) and a deep knowledge of the community’s needs, rely heavily on Safari Doctors.
“Without Safari Doctors coming every month, I would have had to cope with all the medical problems,” said Omar Mohammed, a community health worker who runs a medicine dispensary serving Kiangwe’s scattered huts. The organization’s visits have “made a big difference to people’s health,” he added.
Most of the villagers who come to see the Safari Doctors arrive with common ailments ― coughs, colds, cuts and sores. The medical staff performs routine checkups, then screens for more insidious illnesses.
“I’ve come because my daughter has a high fever,” said Zainab Bakari, a 26-year-old mother of two who spoke to HuffPost. “The doctors here helped my son last year, so I’ve returned with my daughter because she is sick.”
This time, the doctors say it is a stomach infection that will soon clear. But Bakari was right to worry: The area has seen outbreaks of dengue fever and chikungunya, mosquito-borne diseases that can be fatal. There is also the risk of elephantiasis, a painful and disfiguring parasitic disease that causes body parts to swell to unnatural sizes. Even the risk of leprosy remains. Last year, two patients who had the infection got the medicine and were cured, but doctors need to keep a constant eye out for others who may suffer.

It’s important that people have consistent access to health care to have a chance of preventing outbreaks, Kalu said. “You can’t just come to give health care when there is a big outbreak. At that point, it is too late, and you are dealing with diseases as an emergency.”
If one area does not have health care, diseases can spread unchecked to nearby areas.
“Infections do not have boundaries,” said Dr. Monique Wasunna, Africa director of the Drugs for Neglected Diseases Initiative (DNDi), which develops treatments for patients who otherwise might get no help.
“Even in remote areas, there is movement in and out, so the communities around are at risk, too ― even if they have preventive measures and primary health care,” added Wasunna, a tropical medicine specialist who is not connected with Safari Doctors.
Umra Omar, 36, who founded Safari Doctors in 2015, grew up on the Lamu Archipelago and returned after completing her studies in the United States. Even before the militant attacks, medical services were not reaching people in Lamu County who needed them most, she said. A majority of people here live in rural areas, while major health care facilities are in places where the population is denser, she said. The same is true across countries in the developing world. Conflict makes travel even riskier.

For those living in the mainland village of Kiangwe, for example, the road to the nearest hospital frequently washes out in the rain. Getting emergency health care means riding on a motorbike for more than a day, an expensive prospect for the villagers. People who live on the islands must take a boat to the mainland first, an even more time-consuming and costly process.
“Safari Doctors works to fill the gap between the hospitals and health care on the ground,” Omar told HuffPost.
To get all this done, Omar raises funds for medicines and staff salaries from tourism operators, as well as international donors, including the Canadian government. Many of the professionals who work with Safari Doctors are volunteers.
The work they do has a ripple effect that spreads far beyond the Lamu region.
“Prevention is better than cure,” Wasunna said, pointing out that the costs of emergency treatment ― in terms of medication, hospitalization and the effect on patients’ families ― are far higher than having teams like Safari Doctors working to stop diseases in the first place.
“It might seem harder to do, but by putting in place preventive measures, you cover a large population,” Wasunna said. “Then people can lead better lives, and they can contribute to the economy. It helps the development of the country for all.”
If it matters to you, it matters to us. Support HuffPost’s journalism here. For more content and to be part of the “This New World” community, follow our Facebook page.
HuffPost’s “This New World” series is funded by Partners for a New Economy and the Kendeda Fund. All content is editorially independent, with no influence or input from the foundations. If you have an idea or tip for the editorial series, send an email to [email protected].
REAL LIFE. REAL NEWS. REAL VOICES.
Help us tell more of the stories that matter from voices that too often remain unheard.
[ad_2]
Source link

