[ad_1]
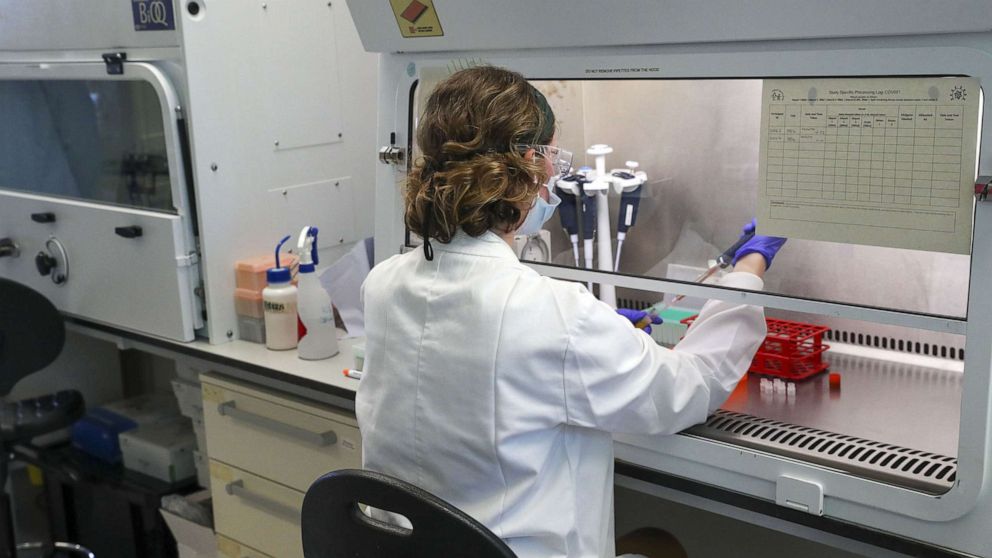
A team of scientists at the University of Oxford released promising results showing their COVID-19 vaccine appears safe in an early-stage study — welcome news for one of the most advanced vaccine programs in the world.
The Phase 1/2 results, published Monday in the scientific journal The Lancet, also showed that the vaccine triggered an immune system response, according to blood samples taken from study volunteers.
“What we’re reporting today is the result of a phase 1 trial in over 1000 people looking at how well this vaccine performs both in terms of its safety, which is good and its immune responses which are pretty exciting,” Professor Adrian Hill, director of the Oxford Jenner Institute, told ABC News.
This finding gives researchers a promising hint at the vaccine’s effectiveness, but experts say only the results of an ongoing, massive Phase 3 study will show if the vaccine really works to protect people from COVID-19 infection.
Nevertheless, researchers were encouraged to see in this Phase 1/2 study that the Oxford vaccine appeared to activate several parts of the immune system. The vaccine was safe, with no serious adverse effects, although some people reported side effects like fatigue and headache.
The University of Oxford has partnered with the pharmaceutical company AstraZeneca, which received a $1.2 billion investment from the U.S. government to help speed up development and ensure U.S. citizens have access to the vaccine should it prove successful.
The Oxford vaccine is one of 23 vaccine candidates currently being tested in studies in people across the globe, according to the World Health Organization.
Two Chinese companies — Sinovac and Sinopharm — have also begun Phase 3 trials. Meanwhile, two other vaccine efforts — one from Moderna and the other from Pfizer and BioNTech — are slated to begin Phase 3 trials this month and have already released Phase 1 results that also appear to be able to trigger multiple parts of the immune system.
The Oxford vaccine uses vaccine technology that contains the virus’s genetic material, but does not actively replicate inside the body, meaning it shouldn’t make people sick.
Instead, it is designed to trigger an immune system response which, once primed, should be ready to attack the novel coronavirus if a person were to be exposed.
By analyzing blood from the more than 1,000 study volunteers, researchers were able to determine that the vaccine seemed to cause their bodies to produce virus-fighting antibodies, which are proteins released by the body to neutralize invading viruses.
Other vaccines, such as those made by Moderna and Pfizer/BioNTech, also showed their capacity to generate these so-called “neutralizing” antibodies in Phase 1 studies.
Antibodies, however, are not the only part of our immune system. New research finds that among people who have been infected and recovered from the virus, antibodies may fade more rapidly than we had hoped, prompting scientists to take a closer look at T cells, another virus-fighting part of the immune system.
Hill said it’s encouraging news to see “both arms of the immune systems stimulated very strongly by the vaccine.”
According to The Lancet study, the Oxford scientists saw that their vaccine seemed to generate so-called “killer” T-cells, also called cytotoxic T cells because they destroy cells that have been hijacked by viral invaders. There’s another type of T-cell, called helper T-cells, that also may play a role in COVID-19 immunity.
Dr. Paul Goepfert, director of the University of Alabama at Birmingham Vaccine Research Clinic, said generating a killer T-cell response is likely a good sign as it may be the combination of all three — antibodies, helper T-cells, and killer T-cells — that makes a difference in the long run.
He added that it makes sense that Oxford’s vaccine would produce killer T-cells because historically vaccines that use the type of technology can induce killer T-cells.
The focus on T-cells comes as scientists have just begun to learn that the antibody response to this novel coronavirus is not as long-lived as many had hoped, and may fade within a few months in some people.
When it comes to this new virus, scientists are still working to understand exactly what parts of our immune system are likely to protect us long term.
“It’s about the robustness and longevity of the response,” said Dr. Paul Offit, a vaccine expert at the Children’s Hospital of Philadelphia. “What people are worried about that just focusing on antibodies to the spike protein, that it it would be short lived if there were not to be a vigorous T helper response.”
According to Offit, it’s the helper T-cells and antibodies that are more likely to be important factors to long-term COVID-19 immunity.
Ultimately, experts agreed that speculating about the relative role of these different parts of the immune system during these early Phase 1 studies is just that — speculation. Although they may offer interesting insights based on the blood analysis, these early studies are primarily designed to monitor safety.
To gauge whether the vaccines work to protect against future infections, experts caution that we will need to wait for larger Phase 3 studies that are designed to determine effectiveness.
“If we want this vaccine to work, or these vaccines to work, the only way to know that is to do a Phase 3 trial,” said Offit.
For now, Oxford’s Phase 1 data mean its vaccine is on track to be authorized by early 2021, should data from ongoing Phase 2 and 3 trials continue to be positive.
“It’s wonderful to be able to do vaccine development at this speed,” said Hill. “It’s never been possible before to find a new pathogen in January and have a vaccine by the end of the year.”
Hill said he’s hopeful that Phase 3 results will be available by the fall. If the vaccine is ultimately authorized, the first to be vaccinated will likely be society’s most vulnerable members, such as the elderly, as well as front-line workers.
“We feel that there’s urgency and pressure really every day so people are working day and night, they’re working weekends,” said Hill. “We’re not going to stop until we get an answer.”
[ad_2]
Source link