[ad_1]
Right now, testing is not accurate enough to use alone to make most decisions, including who should go back to work or to school, the team at the University of Minnesota said.
“It’s a mess out there,” Mike Osterholm, head of the university’s Center for Infectious Disease Research and Policy (CIDRAP), which issued the report, told CNN.
The number of tests that have been completed — numbers widely reported by states and by the White House — show only part of the picture, the report reads.
“The data is really kind of screwed up,” Osterholm said. “It’s because the public health system is overwhelmed.”
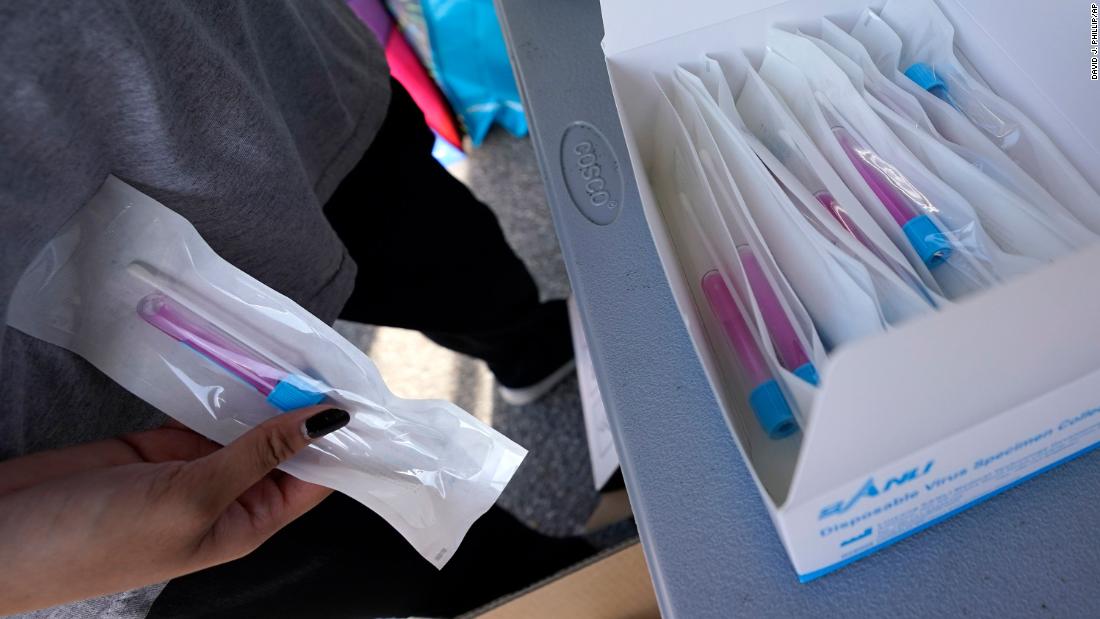
The report has some specific recommendations for diagnostic tests that check to see if someone is currently infected with coronavirus.
Testing is most useful for clinical care of patients, for disease surveillance and contact tracing and for monitoring frontline workers such as emergency responders, doctors and nurses who may have been exposed, the report recommends. People with symptoms should also be tested, it says.
But coronavirus testing is not accurate enough yet to use in many other ways, the CIDRAP team said.
It recommends against:
• Universal testing in hospital settings
• Testing in schools or other low-risk settings
• Widespread community-based testing
• Antibody tests to decide who goes back to work
• Immunity passports
It might be useful to test asymptomatic people in long-term care facilities in some cases because they are likely to have many cases, the report said. “Asymptomatic shedding of the virus may be detected with a molecular test (which looks for the virus itself) or an antigen test (which looks for an immune response to the virus). It is not yet clear where, when and how asymptomatic individuals should be tested.”
The report also says that antibody tests should be used only with caution. These tests check the blood for evidence of an immune response to the virus, and indicate that someone has been infected for some days or has even cleared an infection. They are most useful for identifying donors of plasma used to treat patients or for deciding on how to manage patients when standard diagnostic tests are negative, the report says.
It’s not clear if antibody tests are useful for testing of health care workers to determine immune status, according to the report.
“We believe that greatly expanding SARSCoV-2 testing is a critical element in our response to COVID-19,” the report reads. “For testing to be maximally effective, coordination across the system and across jurisdictions is necessary. Ideally, this requires federal guidance, leadership and support, with strong jurisdictional buy-in at the state and local levels.”
The report calls on the US Department of Health and Human Services to appoint a panel to oversee and organize testing. “The panel should include representatives from public health, clinical laboratory, and medicine; the laboratory testing research and development, marketing, and product support industries; ethicists; legal scholars; and elected officials,” it says.
Osterholm noted that some states are combining data from diagnostic tests and antibody tests to make estimates about how many people have been infected. The Food and Drug Administration advises against using tests in this way and so does Osterholm. “You need to do the right test at the right time to get the right result,” he said. “Nobody is thinking through that.”
Plus, there’s not enough coordination to ensure that states have the testing supplies they need. This is a system and if a system breaks down anywhere, it breaks down everywhere,” Osterholm said.
“What good are the test results if you can’t trust them?”
[ad_2]
Source link