[ad_1]
When the influenza pandemic struck America in 1918, most cities responded with measures that included closing schools.
Yet three cities — New York, Chicago and New Haven, Connecticut — vowed to remain open.
The schools had extensive public health programs in place and argued that keeping students in school was “an opportunity to implement the public health strategies of school medical inspection and intensified disease surveillance,” according to a public health report published in 2010.
Now, more than a century later, as society faces the same question of whether to reopen schools during a pandemic, experts warn that what allowed those three cities to stay open in 1918 is no longer viable.
Dr. Howard Markel, a co-author of the report and a distinguished professor of the history of medicine at the University of Michigan’s School of Public Health, told ABC News that the situations “differ in a billion ways,” namely that there is still little known about the coronavirus and there is no longer an emphasis on public health in schools.
“There was a system in place that has long been dismantled,” Markel said.
In New York City, then-health commissioner Dr. Royal S. Copeland had relied almost entirely on isolation and quarantine to stop the spread of the virus, but was eventually convinced to keep schools open by Dr. S. Josephine Baker, director of the Department of Health Bureau of Child Hygiene, according to the 2010 public health report.
Baker, a leading reformer in the Progressive era, when officials and experts put more of an emphasis on expanding public programs in health and education, believed that many students would be safer in school than out.
At the time, 75% lived in tenements with crowded and unsanitary conditions that made it easier for infections to spread, according to the report.
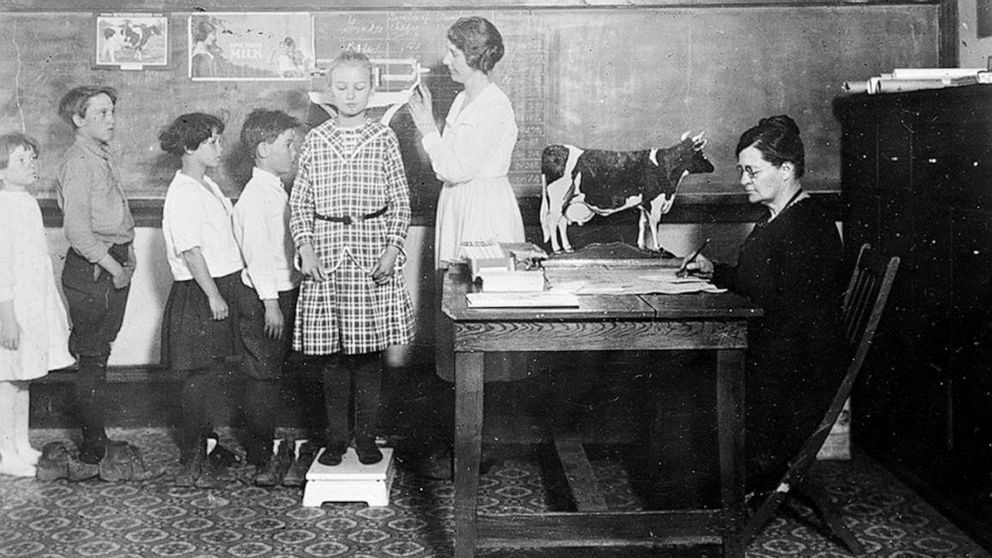
In the schools, students underwent routine inspections, the report noted. Teachers looked for signs of a respiratory condition, such as runny noses, red eyes, sneezing or coughing.
If students displayed any symptoms, they were moved to an isolation room where they were inspected by a health professional and, if feverish, sent home or to a hospital if their home was a potential hotspot for spread.
In Chicago, the city’s health commissioner, John Dill Robertson, believed the schools would be able to build off their “already well-developed school medical inspection program,” according to the public health report.
Robertson coordinated with Dr. C. St. Claire Drake, the state director of health, on a regular basis to develop regulations and plans of action. School health officers and nurses also visited the homes of students who were absent and informed the families of proper procedures for isolation and care.
Chicago suffered greater absenteeism than New York City, which Robertson attributed to “fluphobia.”
New Haven’s health officer, Dr. Frank W. Wright, also was among those who urged schools to remain open.
Wright argued that children would “be safer in the well-ventilated schools where physicians and nurses worked full time to identify sick children and send them home for proper care,” according to the 2010 report.
In early October, about a month after the pandemic struck, health and school officials agreed children should stay in school to keep them from congregating elsewhere without supervision and to minimize their exposure to infected adults.
Markel and another co-author of the report, Dr. Alexandra Stern, made a point to note that the influenza outbreak and novel coronavirus outbreak are not the same epidemiologically.
Though the 1918 outbreak was severe, health experts knew much more about influenza than they do now about the novel coronavirus — and its effects on children.
A recent study out of South Korea found that children younger than 10 years old transmitted COVID-19, the disease caused by the respiratory virus, to others much less often than did adults, although the risk is not zero. Those aged 10 to 19 spread the virus at about the same rate as adults, according to the study.
Another study out of the United Kingdom found that children younger than 18 were not as adversely affected by COVID-19 as adults.
Markel put it simply: “The key word in this novel coronavirus is ‘novel.’ It’s new.”
The U.S. Centers for Disease Control and Prevention has swayed on reopening schools. Originally, the federal agency warned of the risks that come with reopening schools and issued recommendations. But on Thursday, two weeks after President Donald Trump demanded schools reopen, the CDC shifted its tone and released statements about children not being at a high risk of getting seriously ill, though its original guidance still remained on its website.
Markel also said that detailed responses like those available in 1918 would be unlikely or just not possible today because so much funding has been cut for public health programs.
“Over the past several decades, financial cutbacks to public education have severely impacted public health programs, reducing the number of school nurses and resources for activities such as physical education,” according to the 2010 study.
Stern called most public schools “woefully underfunded,” with most having “one rotating nurse who will move between five public schools.”
“The bottom line is that the public health infrastructure that was built into schools as they expanded in the early 20th century has been chipped away at and dismantled to a great extent,” Stern said.
As of 2018, the most recent data available on school nurses, there were 95,776 working full time across the U.S., according to the National Association of School Nurses. With around 50.8 million students in public schools, that is about one nurse for every 530 students.
Statistics like this show how difficult it would be for routine medical inspections, let alone practices adopted in Chicago like how nurses visited the homes of absent students.
Markel and Stern, however, acknowledged the complexity of the issue, saying that for many children school is not just a place for education.
“The best reasons, or the most compelling reasons, of wanting kids to go to school is that they live in an unsafe environment — and school nutrition,” Markel said, though he noted some school districts have vowed to deliver meals.
He’s of the mindset that school is “not a good idea right now.”
Stern felt similarly, saying there are “so many unanswered questions.”
“And when there are unanswered questions about a deadly virus,” Stern added, “one could argue that it makes most sense to follow the precautions principle, which is, ‘Do the least harm.'”
[ad_2]
Source link