[ad_1]
Now, some are sharing what it’s like inside their hospitals as they face an unprecedented crisis. Some are overwhelmed, they told CNN, and others are afraid. Their hearts break for their patients and their patients’ families.
Here’s what they have to say.
“The number of Covid patients we are getting is rapidly increasing every day and all of us collectively worry about what will happen as it gets worse if this is where we are starting,” said the nurse, who asked not to be named for fear of reprisal.
And she’s not the only one who’s afraid, she added.
“When I was working on the Covid unit, some nurses did not want to eat or drink for 12 hours because they were scared to take off and put on the same PPE (personal protective equipment),” she said.
It’s been hard, she said, to see the toll the coronavirus takes on families who are unable to visit their loved ones in the hospital.
“It’s extremely heartbreaking for the families of these patients to have to stay at home while their loved ones fight for their lives,” she told CNN. “It’s brought me to tears a few times updating family on the phone and hearing their frustrations just hoping their family member will start to get better soon.”
University of Chicago Medicine has not responded to CNN’s request for comment.
‘I cried the entire ride home’
In a social media post Wednesday, one nurse at a large Long Island hospital in New York shared her feelings on social media, saying, “I haven’t slept because my mind won’t shut off.”
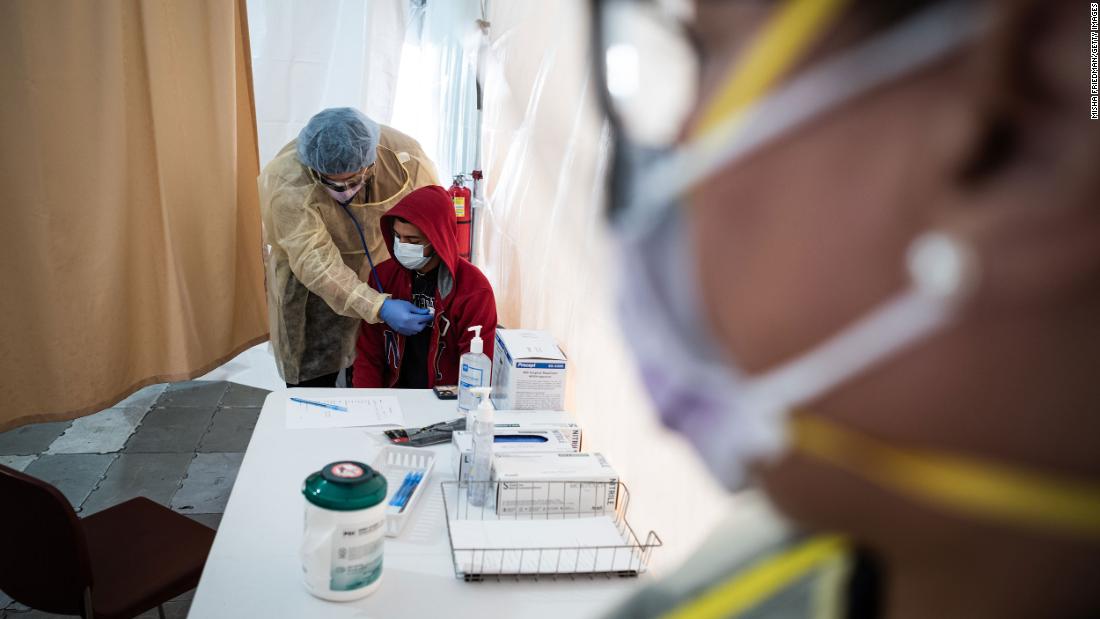
The nurse, who said she works in a Covid-19 triage area, said the previous night was “so far the worst I have seen.”
Patients were streaming in nonstop, she said, coughing and sweating, with fevers and “fear in their eyes.” The nurse wrote that she cried in the bathroom during her break, peeling off the PPE that left indentations in her face.
“I cry for my co workers, because we know it will get worse and I already feel like that is impossible and we are already at our breaking point,” she said. “I cry for the parents, children, siblings, spouses who cannot be with their loved ones who may be dying but can’t have visitors because there is no visiting allowed.”
“I am begging you to stay home,” she wrote. “Please. I cannot stay home and if you do not listen this will not end. It looks like a movie but it’s real life and I cannot believe its real.”
‘I may be the last face they see’
Dr. Cory Deburghgraeve, an anesthesiologist at the University of Illinois in Chicago, said he’s working 94 hours this week. He’s the designated “airway anesthesiologist” giving coronavirus patients breathing tubes in a procedure called intubation.
Deburghgraeve shared a video with CNN of him donning his PPE, putting on gloves, a protective gown, a face mask and then another mask that looks like a space helmet.
Intubation, he said, is considered a high-risk procedure “because we are so close to the patient’s mouth while placing the tube and they often cough up secretions which releases virus into the air we breathe.”
Deburghgraeve said he and his colleagues have been “shocked” at the ages of some of their patients. He’s had several in their 30s, 40s and 50s, he said. The coronavirus, he warned, doesn’t just affect older people.
“What’s very devastating for me is some people we know will not survive,” he said, “and since they’re not allowed to have visitors, I may be the last face they see and voice they hear ever as I put them to sleep (general anesthesia) prior to being on a ventilator.
“So, despite being busy … I try to show extra compassion, extra emotion, try to hold their hands and as much as I can (have) human connection, despite the fact that I’m wearing what looks like a space suit.”
Hard to move in cramped conditions
An emergency room physician at a hospital in the New York borough of Queens said doctors and nurses must deal with cramped spaces.
“Stretchers are packed in metal-to-metal, stacked three deep head to toe, with no space … to walk to patients,” the physician said. “When patients deteriorate, you hope you see them from across the room and hope you can move enough stretchers out of the way to get that person to a critical care area.”
The doctor added that “critical care patients are stuffed into the critical care area with patients floating in the middle of the room,” and that some admitted patients are sitting in chairs because they do not have any more free stretchers, and there is no room.
The physician said the availability of portable oxygen tanks is a concern. “We are in danger of running out of those tanks every day,” the doctor said.
‘Everything is not fine’
At Elmhurst Hospital in New York, health care workers are living in a “constant state of paranoia,” according to one person who identified as a nurse there but did not want to be named.
“We don’t know if we even have the virus,” the person said, “and we’re so scared to give it to someone else.”
At least 13 people died at the Queens hospital within a 24-hour period, according to a Wednesday statement from NYC Health and Hospitals/Elmhurst. The hospital is “at the center of this crisis,” the statement said, and the staff is “going above and beyond” to address it.
Smith shared footage from inside the hospital, of hospital beds and a room she said was filled with coronavirus patients. Outside the building, a refrigerated truck was being used to store the bodies of patients who died, she said.
“I don’t have the support that I need, and even just the materials that I need physically to take care of my patients,” Smith said. “And it’s America and we’re supposed to be a first-world country.”
CNN’s Shimon Prokupecz, Jasmine Wright, Paul P. Murphy, Laura Dolan, Brynn Gingras, Linh Tran and Curt Devine contributed to this report.
[ad_2]
Source link